Understanding Egg Allergies in Babies
Egg allergy always refers to a hen’s egg allergy. It is the second most common food allergy in infants and young children, affecting anywhere from 1% of babies in the United States to 9.5% of babies in Australia!
The good news is that a large percentage (~80%) of children will outgrow an egg allergy by age 5. The bad news is that for those first 5 years, a child with an egg allergy has to be very, very careful about what they eat.
Egg Yolk Allergy, Egg White Allergy, and Heated Eggs
Egg allergy is an immune system response to one or more proteins in an egg. Egg allergy can cause an immediate allergic reaction, as well as longer lasting eczema and reflux (heavy spitting up) symptoms in babies.
Egg White Allergy
The most common egg proteins that babies are allergic to are found in the egg whites, meaning most babies actually have an egg white allergy. There are two proteins in egg white that cause allergies:
- Ovalbumin (OVA), also called Albumin / Albumen
- Ovomucoid (OVM)
Note: People can also be allergic to other egg white proteins like ovotransferrin, ovomucin, lysozyme, and ovoglobulin, but these specific egg white allergies are rare.
Heated Egg: Baked or Hard-Boiled
The ovalbumin protein in egg whites is heat sensitive. If eggs are boiled for 15 minutes in water, most of the ovalbumin protein breaks down. If eggs are baked (mixed with starch and heated at 350 F for 30 mins) all the ovalbumin breaks down. This means babies who are only allergic to ovalbumin can eat baked eggs, because there is no un-borken ovalbumin left in a baked egg.
Egg Yolk Allergy
The egg yolk, on the other hand, is made of totally different proteins, which do not seem to cause allergies very often. Some protein from the white can get into the yolk and vice versa, but very few babies have an egg yolk allergy.

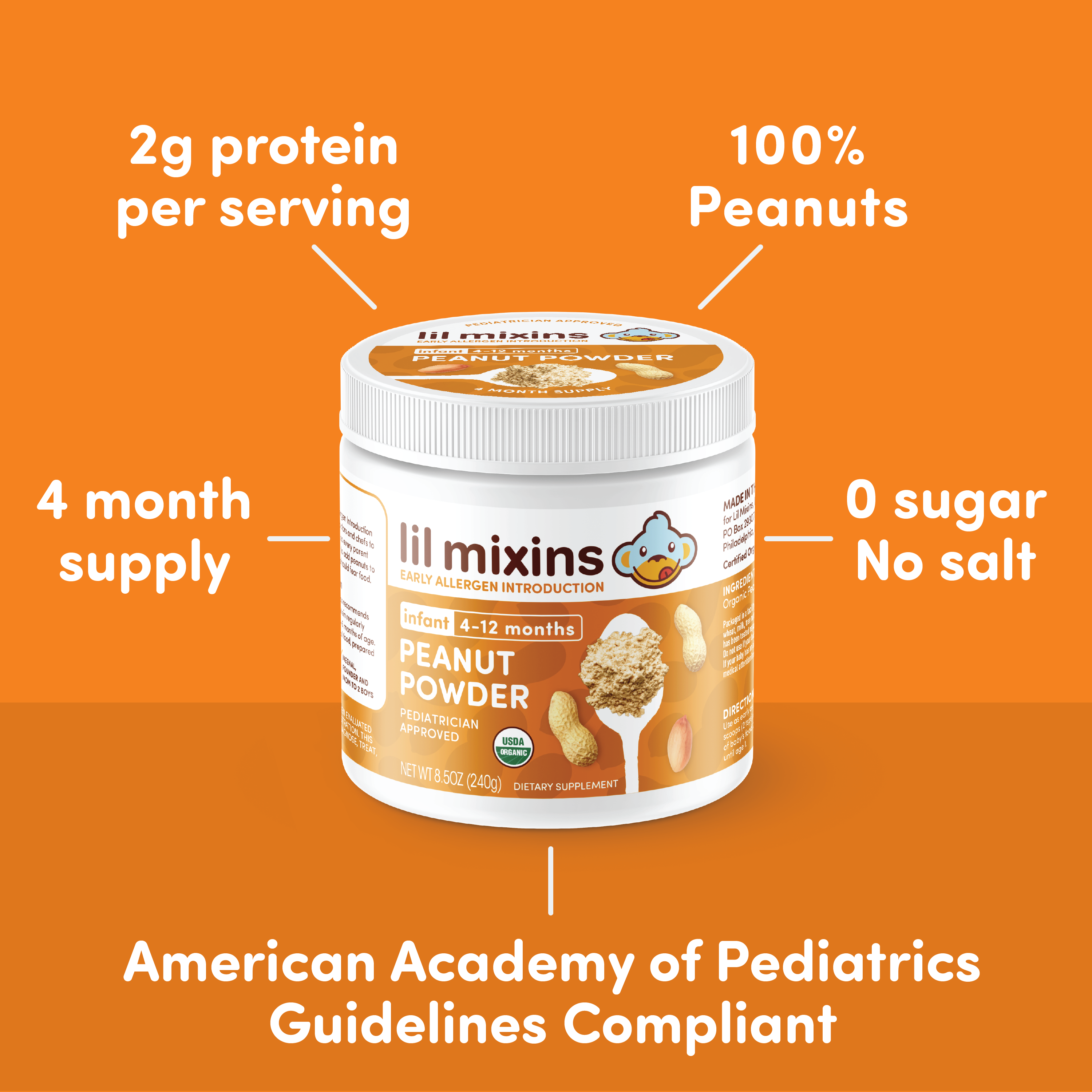
Shop Hardboiled Egg Mixin 4-Month Supply
Testing for Infant Egg Allergy
The five important proteins in hen’s egg are labeled Gal d 1 to 5 (from the latin name Gallus domesticus) . Egg whites contain ovomucoid (Gal d 1), ovalbumin (Gal d 2), ovotransferrin (Gal d 3), and lysozyme (Gal d 4). Chicken serum albumin (Gal d 5), is in the egg yolk protein.
Blood, or specific IgE testing, can identify which proteins a person is allergic to. This can predict if a child can safely eat baked egg, or perhaps even cooked eggs. But only an oral food challenge can determine a true allergy.
Skin testing for egg allergy may also be important. Stomach acids break down egg proteins, so some people may react to touching an egg, but not to eating it.
Egg Allergy, or Something Else?
An IgE egg allergy is usually easy to spot. The reaction will begin within minutes of eating egg, and the symptoms will look like hives and vomiting / diarrhea in babies, and wheezing, runny nose, and coughs in older children.
However, it is possible to have an egg allergy based on immune cells other than IgE. While we don’t understand these allergies nearly as well, doctors have found that egg allergy can cause delayed symptoms like persistent eczema and eosinophilic esophagitis (usually called EoE).
Egg allergy can also cause food protein-induced enterocolitis syndrome (FPIES) which will look like regular vomiting and has daily runny poops.
Talk to your doctor if you are seeing these symptoms.
Outgrowing an Egg Allergy
Like cow’s milk allergy, almost 80% of children seem to naturally outgrow an egg allergy. Being able to eat baked egg, and regularly eating it seems to increase the chance of outgrowing an egg allergy.
As with all allergies, kids with lower levels of IgE antibodies and fewer other allergic diseases are more likely to outgrow an egg allergy.

Shop Daily Mix One-Month Supply
Preventing an Egg Allergy
After peanut allergy, the possibility of preventing egg allergy is the most studied and proven.
Across five different studies, and most recently the PETIT study, it has been shown that most egg allergies can be prevented by feeding babies eggs as soon as they can tolerate solid foods.
Starting with hard-boiled egg was shown to be 15 times safer for young babies than starting with scrambled eggs. Because most babies are allergic to egg whites, feeding babies egg yolks was not found to be helpful because the proteins needed for immune training are in the egg whites. Babies should never be fed raw eggs.
Lil Mixins Hard Boiled Egg Powder and Daily Mix with Hard-Boiled Egg eliminates the time it takes to cook eggs, and makes them safe for babies as young as 4 months old.